
Ade Williams/The Pharmaceutical Journal
After reading this article, you should be able to:
- Increase your understanding of the factors contributing to men’s health inequality;
- Appreciate the importance of intentionally creating a male-friendly pharmacy practice culture;
- Identify and create simple, effective solutions that exemplify an approachable, inclusive healthcare environment;
- Adopt co-design approaches when delivering and evaluating health equality.
Introduction
While gender-defined roles and societal expectations for gender equality have advanced significantly over time, it is undeniable that misogyny and gender-based imbalances continue to persist in the UK. Within this context, the health challenges faced by men is a further societal problem that needs to be urgently tackled.
One in five men die before the age of 65 years[1]. In England and Wales, 17.5% of all male deaths are between the ages of 15 and 65 years, equating to 748,000 years of life lost when compared with the national life expectancy[2]. It has been further estimated that 28% of male deaths are preventable[3].
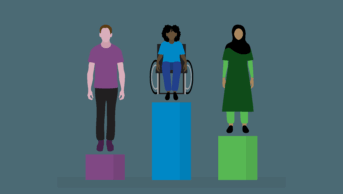
In the UK, there is a ten-year difference in life expectancy for men depending on where they live, primarily owing to poverty[4]. Many of the health challenges men face are markedly affected and amplified by the social determinants of health and intersectional factors, with socio-economic pressures, ethnicity, disabilities, along with gender and sexual minority status, all being associated with a greater risk of health inequality.
Pharmacists, particularly those in community pharmacy, are uniquely positioned to lead local interventions that target these inequalities and positively influence the health of men in their local area. This article will provide a series of tips and examples that demonstrate ways pharmacists can engage in men’s health promotion. It is based on the experience of our community pharmacy in Bedminster, South Bristol, where significant efforts have been made to champion men’s health.
Barriers to accessing primary care
Before considering how to provide effective health promotion targeted at men, it is necessary to understand the fallacy of assuming men will step forward to seek health advice when needed. In 2021, Peter Baker, director of UK charity Global Action on Men’s Health, claimed that there are two main barriers to men’s effective use of primary care[5]. First, some men see seeking help as undesirable because it feels challenging to traditional notions of masculinity. The gender norms that inhibit many men include their need for independence and control and their unwillingness to show vulnerability or “weakness”. Many men endure pain and downplay symptoms to adhere to masculine norms.
The second barrier is more practical: relatively few services are targeted at men or delivered to meet men’s needs. Men often find conventional primary care services difficult to access. For example, appointments may not be available at times that are possible because of work commitments, and traditional gender imbalances and roles within families may still result in many men subordinating healthcare. In the author’s professional experience, men rarely complain about waiting on the phone to get a GP appointment; they either do not try or never stay in the queue. Even worse, many from minority communities, sometimes owing to their employment status and job roles with less flexibility, have never joined the 8.30am appointment rush. It is not an option open to some — a previously identified socio-economic barrier that intersects with race[6].
Baker professes solutions to the two barriers highlighted: first, he suggests making primary care services more accessible to men by removing obstacles, such as broadening open hours, and by utilising digital technologies for making appointments and accessing information, advice and consultations. He also suggests delivering services in settings where men feel more comfortable, such as workplaces, faith, sports and other leisure venues[5].
Designing initiatives to address men’s health inequalities
To address health inequalities, it is important to understand the specific health dynamics of your local area. Local population data can be analysed and may reveal specific social determinants of men’s health inequality, another facet of social injustice.
Several initiatives in the Bedminster pharmacy were designed to address men’s health inequalities in the local area. The following examples describe the approach taken and can be easily adapted or replicated to fit local needs.
Example 1: creating an inclusive environment
While this may sound like a simple objective on the surface, it requires concerted effort and careful consideration to achieve a welcoming environment for all genders.
Community pharmacy is one of the most frequented healthcare settings in England, with 1.2 million health-related visits each day[7]. However, there is a significant qualitative difference between men who fully engage with the range of wellbeing opportunities and health expertise provided by the pharmacy and those who wait patiently in the queue, and exit as fast as possible.
This approach began by engaging with a cross-section of male patients, six agreed to audit the pharmacy, with the aim of identifying and suggesting ways to make things more accessible and welcoming to men.
Simple actions from this audit included:
- Improving signage so that it was clear that the patient’s request to speak with either a male or female team member is welcome and considered;
- Improving signposting informing patients of the availability of a private consultation room for conversations or queries. Bedminster pharmacy has two consultation rooms, one right beside the main door; however, only two out of the six male patient auditors could recall ever noticing the sign on the door.
This simple improvement led to a significant increase in requests by men to use the consultation rooms. On reflection, this makes logical sense: if you are entering an unfamiliar space and less in control, for some, discussing your health within earshot of other patients can be terrifying. While many patients feel comfortable sharing such details at the counter, privacy and dignity are yardsticks of excellent clinical pharmacy practice.
Example 2: men’s health messaging within the pharmacy
Pharmacies should take every opportunity to promote good health and it is good practice to think creatively about the most effective ways to deliver health promotion messaging. It is possible to create targeted messaging on men’s health; for example, deploying in areas where male grooming products are kept. Putting up posters and leaving out a nice pile of leaflets is unlikely to be the most effective way of engaging patients. After all, if you do not feel you have health vulnerabilities, why would you do a faecal immunochemical test for bowel cancer or check your blood pressure regularly, even if you have a strong familial link to cardiovascular incidents?
Examples of targeted approaches taken include the pharmacy’s annual week-long ‘Bemmy Challenge’. Coinciding with men’s health week, the campaign challenges men in the local area to face up to their health risks and come in for cardiovascular risk assessments, weight, height, blood pressure and waist measurements during the week. Partnering with local media helps to promote the message and patients who complete the challenge receive a token gift and a challenge-stamp tattoo, badge or sticker. The critical objective is to communicate what the scores mean and promote the help pharmacy can provide in relation to lifestyle modification, such as reducing alcohol intake, smoking reduction, increasing physical activity, weight loss, diet change and signposting, where appropriate, to a medical practitioner.
Example 3: outreach and working within the community
Another way of targeting men’s health promotion interventions is to work beyond the pharmacy. The Bedminster pharmacy holds a regular weekly blood check clinic, ‘Pulse in the Pub’ that aims to demystify healthcare professionals and serve members of the community who may not be regularly accessing primary care. This intervention was initiated after a throwaway comment was made by a trainee pharmacist colleague who asked the question: “Why are we setting up blood pressure clinics in the pharmacy? We need to go where the people who never come here are!”.
‘Pulse in the Pub’ has become one of the most engaging, insightful and culture-shaping interventions Bedminster has developed. To learn more about this initiative, listen to the ‘Building bridges: pharmacists reaching out to help their communities’ episode of The PJ Pod.
The value of the clinic goes far beyond the readings taken on the day. As healthcare professionals, by placing ourselves where some male patients feel most relaxed and comfortable, it removes any necessity or need to manage any potential power imbalance. This also removes the perception that healthcare professionals are figures of authority, but instead the motives of trying to help and making a positive difference are recognised.
This initiative results in follow-up appointments in the pharmacy for the hypertension case finding service promotes discussions about other health and wellbeing concerns, but better still, patients decide to bring a friend with them to engage in conversations with the pharmacy team about their health. When patients start to tell their peers about the social merit in having a good relationship with the most accessible part of the NHS, this presents pharmacists and pharmacy with a fantastic opportunity to make a significant difference.
Consultation skills
It is also important to invest in communication skills and learn how to deliver the correct type of inclusive and effective consultations. Patients do not like feeling dispossessed of autonomy, especially when dealing with health concerns. Every effort should be made to ensure appropriate language is used, entering into shared decision-making with informed consent, providing opportunities to discuss the evidence and consider options so that interventions are shaped around the patient’s wishes, even if there is a clinical urgency to make an evidence-based choice. Trust also builds emotional safety, so these consultations create opportunities to discuss mental health, work-related stress and relationship pressure.
Box: Viagra POM-to-P switch
One of the most significant dividends of the generic viagra sildenafil POM-to-P switch was the opportunity for men to receive structured clinical care in the privacy of the community pharmacy. The focus on the link between erectile dysfunction and cardiovascular disease also creates an opportunity for exploratory conversations with pharmacists. For some, this could be the first-time they experience the breadth of expertise and depth of clinical knowledge that their local pharmacy has to offer increasing the likelihood of their positive engagement in the future.
Understanding the demographics and cultural context of your local area
Another critical action is to understand the demographic makeup of your male population. This can include looking at age, socio-economic status, ethnicity, educational attainment level and the languages most commonly spoken. Any campaigns or information sharing must consider this context and it usually requires a concerted effort to create appropriate tools that can engage local communities creatively. It is important not to underestimate the benefits of drawing on the local character of your area. This can include local sport club allegiances. For example, staff in the Bedminster pharmacy wear the colours of both Bristol City football clubs, which they say helps to send a message that they are part of the community and can be an effective tool for establishing rapport with men who follow football. They say they are frequently asked by patients: ‘Which one do you support then — City or Rovers?’.
Community pharmacy can also help to target national health campaigns to the local male population; for example, by increasing uptake of COVID-19 and flu vaccinations, signposting into local social prescribing pathways for support with social isolation, accessing targeted social security support and alleviating loneliness and social isolation.
Advocating for men’s health
When developing interventions targeting men’s health, inspiration can be taken from international examples. Australia now has had one of the most ambitious and best articulated men’s health strategies, launched in 2020 and building on years of work, tackling the gender-based health inequity that only worsens with ethnicity and socio-economic status[8]. The strategy is an exemplar and a rich source of guidance, much of which can be applied to the UK context.
In November 2022, the Men’s Health Forum led a coalition of organisations to campaign for a Men’s Health Strategy, highlighting why it will help promote men’s health equity as well as the missed opportunity to align this with the ‘Women’s Health Strategy for England’, published by the UK government in 2022[9].
There is a clear and pressing need to address men’s health equity, with community pharmacy central to any effort to do so. Men’s health promotion is a rewarding but challenging endeavour that all healthcare professionals need to engage with. By adopting a proactive approach, only made possible with sustainable funding and opportunities to deliver timely, relevant clinical interventions that build on our accessibility offer, we can make a significant difference.
Best practice
- Invest time to research and understand your local male population health profile;
- Create a team-owned approach to delivering men’s health equity;
- Embed quality improvement methodology in your work, so you can continually evaluate, learn and improve any initiatives you develop;
- Invite your community to help with evaluating and co-designing your pharmacy services to enshrine equity and broad access.
SPONSORED FEATURE: Phosphodiesterase 5 receptor (PDE5) inhibitors and the treatment of erectile dysfunction
Article commissioned and fully funded by Sanofi Consumer Healthcare
- 1Key Data: mortality. Men’s Health Forum. https://www.menshealthforum.org.uk/key-data-mortality (accessed Jul 2023).
- 2White A, Tod M. The need for a strategy on men’s health. Trends Urol & Men’s Health. 2022;13:2–8. doi:10.1002/tre.842
- 3Marmot M, Allen J, Boyce T, et al. Health Equity in England: The Marmot Review 10 years on. Institute of Health Equity. 2020.https://www.instituteofhealthequity.org/resources-reports/marmot-review-10-years-on/the-marmot-review-10-years-on-full-report.pdf (accessed Mar 2023).
- 4Major study outlines wide health inequalities in England. The Health Foundation. 2022.https://www.health.org.uk/news-and-comment/news/major-study-outlines-wide-health-inequalities-in-england (accessed Jul 2023).
- 5Baker P. Men and Primary Care: Removing the Barriers. Harvard Medical School Primary Care Review. 2021.https://info.primarycare.hms.harvard.edu/review/men-primary-care (accessed Jul 2023).
- 6Banks I, Baker P. Men and primary care: improving access and outcomes. Trends in Urology & Men’s Health. 2013;4:39–41. doi:10.1002/tre.357
- 7Pharmacy playing a pivotal role in prevention and public health. UK Health Security Agency. 2019.https://ukhsa.blog.gov.uk/2019/06/28/pharmacy-playing-a-pivotal-role-in-prevention-and-public-health/ (accessed Jul 2023).
- 8National Men’s Health Strategy 2020-2030. Australian Government Department of Health. 2021.https://www.health.gov.au/sites/default/files/documents/2021/05/national-men-s-health-strategy-2020-2030.pdf (accessed Jul 2023).
- 9Women’s Health Strategy for England. Department for Health and Social Care. 2022.https://www.gov.uk/government/publications/womens-health-strategy-for-england/womens-health-strategy-for-england (accessed Jul 2023).
1 comment
You must be logged in to post a comment.


I have read and found good knowledge.