Science Photo Library
After reading this article you should be able to:
- Differentiate the types of paediatric-specific prescribing errors;
- Understand why paediatric prescribing errors occur;
- Understand the role of education in the prevention of paediatric prescribing errors;
- Identify the most effective format for feedback relating to paediatric prescribing errors.
Introduction
Paediatric medication errors — more specifically, prescribing errors — are some of the most important threats to patient safety in children[1]. These errors affect around 13% of paediatric prescriptions and can have lethal consequences[2,3]. Evidence suggests that errors occur more frequently in children than in adults and may be up to three times more likely to cause harm[2,4,5].
Despite increasing recognition of this problem — and calls from the World Health Organization to reduce medication-related harm — the goal of improved medication safety in children has not been fully realised[6]. Experts suggest that an in-depth understanding of the nature and causes of errors is essential to underpin improvement, but they highlight the lack of specific studies in children required to enact change[7,8]. This is especially important because evidence for the causes of errors in adults does not reflect the significant differences in paediatric medication use.
Pharmacists play a primary role in supporting safe prescribing, including identifying errors; guiding prescribers; giving feedback; delivering education; and leading quality improvement initiatives[9–12]. These roles are more likely to be effective if informed by detailed evidence about prescribing errors and their underlying causes.
This article aims to help improve the safety of prescribing for children by reviewing evidence showing causes of errors and outlining potential solutions. It is intended to be relevant to practitioners in both primary and secondary care; although, given that most research has been conducted in secondary care, it is acknowledged that this setting is emphasised. The article is composed of two main sections. The first summarises the nature of paediatric prescribing errors, systemic frameworks for understanding error causation, and up-to-date evidence about how they happen. The second section covers supporting safer prescribing, using information about error causation to review how pharmacists can promote safer prescribing for children, with a specific focus on prescribing education and feedback.
The prescribing process
As part of a chain that includes dispensing, administration and monitoring, prescribing is just one element of safe medication delivery. Prescribing is an integrated process with multiple component steps, including:
- Patient assessment;
- Medication choice (via shared decision making with the patient);
- Prescription writing;
- Information provision;
- Monitoring[13,14].
Although prescription writing has been most extensively studied within clinical audit and research, prescribing errors can occur during any of these steps. Published definitions of prescribing error reflect this concept of prescribing, with Ghaleb et al. suggesting that a clinically meaningful prescribing error occurs when a prescribing decision or prescription reduces the probability of treatment being timely and effective, or increases risk of harm when compared with generally accepted practice[15,16]. While much of the evidence discussed within this article relates to errors in prescription writing, the authors advocate the use of a broad definition of error, which encompasses other aspects of prescribing — for example, medication choice or communication with patients — because this approach offers the greatest potential to improve practice.
The nature of paediatric prescribing errors
Practitioners aspiring to improve prescribing safety first require background knowledge of the nature of errors affecting children. This section summarises the different types of prescribing errors and the harm they can cause, as well as evidence showing their frequency and high-risk aspects of practice.
Epidemiology and harm
Paediatric prescribing errors are common, with a UK multicentre study identifying errors (using the above definition) in 13.4% of ‘medication orders’ (written prescriptions on medication chart review) in hospitalised children[2,16]. One primary care study found that, within a one-year period, 26.1% of children in primary care received an off-label prescription. Prescribing off-licence is not an error in itself; however, the authors suggested that 75–85% of these prescriptions were associated with error relating to incorrect dosing, implying that up to 22% of children in primary care may have received an incorrect prescription[17].
Most errors are intercepted prior to or during administration and do not impact patients, in which case practitioners may not choose to use the error as an opportunity to improve practice[18,19]. When errors do reach patients, they often do not lead to harm because the patient is able to tolerate the error without experiencing adverse effects (e.g. a baby receives a double dose of paracetamol but suffers no ill effects)[20]. This offers limited reassurance because the overall prevalence of error is so high that many serious errors do occur[2,3]. Moreover, the most severe errors have catastrophic outcomes: a study of published UK newspaper articles identified 29 fatal paediatric medication errors that have been reported on over an eight-year period[3].
The economic burden of prescribing errors is significant. A recent analysis estimated that 66 million potentially clinically significant medication errors occur in England annually, with an associated cost of £98m[21]. Studies involving medication in children contributed to this estimated cost; however, it is not possible to know what proportion of this figure accounts for paediatric care specifically[21].
Errors have human costs that are difficult to quantify and receive little attention in research. These include emotional damage to patients and families, and loss of trust in the healthcare providers involved. Prescribers, dispensary staff and those involved in administration suffer distress and anguish from involvement in errors, and there are associated long-term psychological impacts[22].
Error types
Ghaleb et al. found that 41% of errors in paediatric hospital inpatients resulted from incomplete prescriptions and 24% from inappropriate use of abbreviations[2]. Many are included on the National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) dangerous abbreviations list[23]. Errors such as these (e.g. abbreviating micrograms to ‘mcg’) may have a particular impact in children because pharmacist unfamiliarity with paediatric dose ranges could make detection more difficult[24].
Dosing errors have repeatedly been found to be the most common prescribing error in children[25,26]. This includes tenfold dosing errors — those in which a dose is incorrect by a factor of ten — which can be lethal[27]. This is likely because of the high reliance on individualised (e.g. weight-based) dosing in paediatrics[24]. Owing to methodological differences between studies, it is unclear whether dosing errors are more common in children than in adults[24].
High-risk groups
Analysing causes of errors can be a complex and time-consuming process, leading to calls for high-risk errors to be prioritised[28]. Risk is a function of the frequency with which an error occurs and the likelihood that it will lead to severe harm[28]. Tools such as the NCC MERP Index for Categorizing Medication Errors may assist in assigning risk, although it may be useful to consider harm that could have occurred, and not just the actual outcome[29]. Whether or not harm results from an error may be influenced by the medication involved, the type and magnitude of the error, the likelihood that the error will be detected, and the age of the patient and their ability to tolerate the error’s effects[5]. This definition of risk implies that both commonly used medications with comparatively low risk of harm and infrequently used, but more hazardous medications can be considered ‘high-risk’ and worthy of prioritisation within medication safety efforts.
A recent analysis of more than 500 prescribing errors found that care for neonates (particularly in neonatal care unit settings), the process of medication dosing, and specific drug types represent high-risk areas of practice (see Table 1)[30]. While it should be noted that under-reporting and biases mean that incident data may not be representative, this evidence suggests that medications implicated in paediatric errors differ from those in adults[31,32]. This finding is likely to reflect different patterns of medication use in children. Medications deemed high risk in adults (according to the Institute for Safe Medication Practices based near Philadelphia, Pennsylvania) that are commonly involved in paediatric errors include opiates, benzodiazepines and insulin[30,33,34]. Children’s size and physiologic immaturity leaves them vulnerable to harm from medications not formally classified as high risk, such as when a neonate receives an overdose of intravenous paracetamol[35].
In many cases, factors that increase likelihood of error may be associated with an increased likelihood of harm[5]. For example, premature neonates are difficult to prescribe safely for, are cared for in pressurised intensive care environments, and are physiologically vulnerable to the effects of errors[5].
Other clinical settings may predispose to errors. Children are a particularly challenging group in whom to use medications safely; therefore, receiving care in non-specialist paediatric settings might increase risk of error, owing to staff having less experience prescribing for children and reduced access to resources such as paediatric pharmacist support[35,36]. However, there is little empirical study to support this theory, with settings such as primary care, where children receive a high volume of care, underrepresented in current research.
How paediatric prescribing errors happen
To prevent errors, healthcare first needs to develop a culture that views error as a systemic problem, in which practitioners’ contributions to error causation are considered as part of their wider working context. Several frameworks exist to support practitioners in elucidating errors’ complex underlying causes.
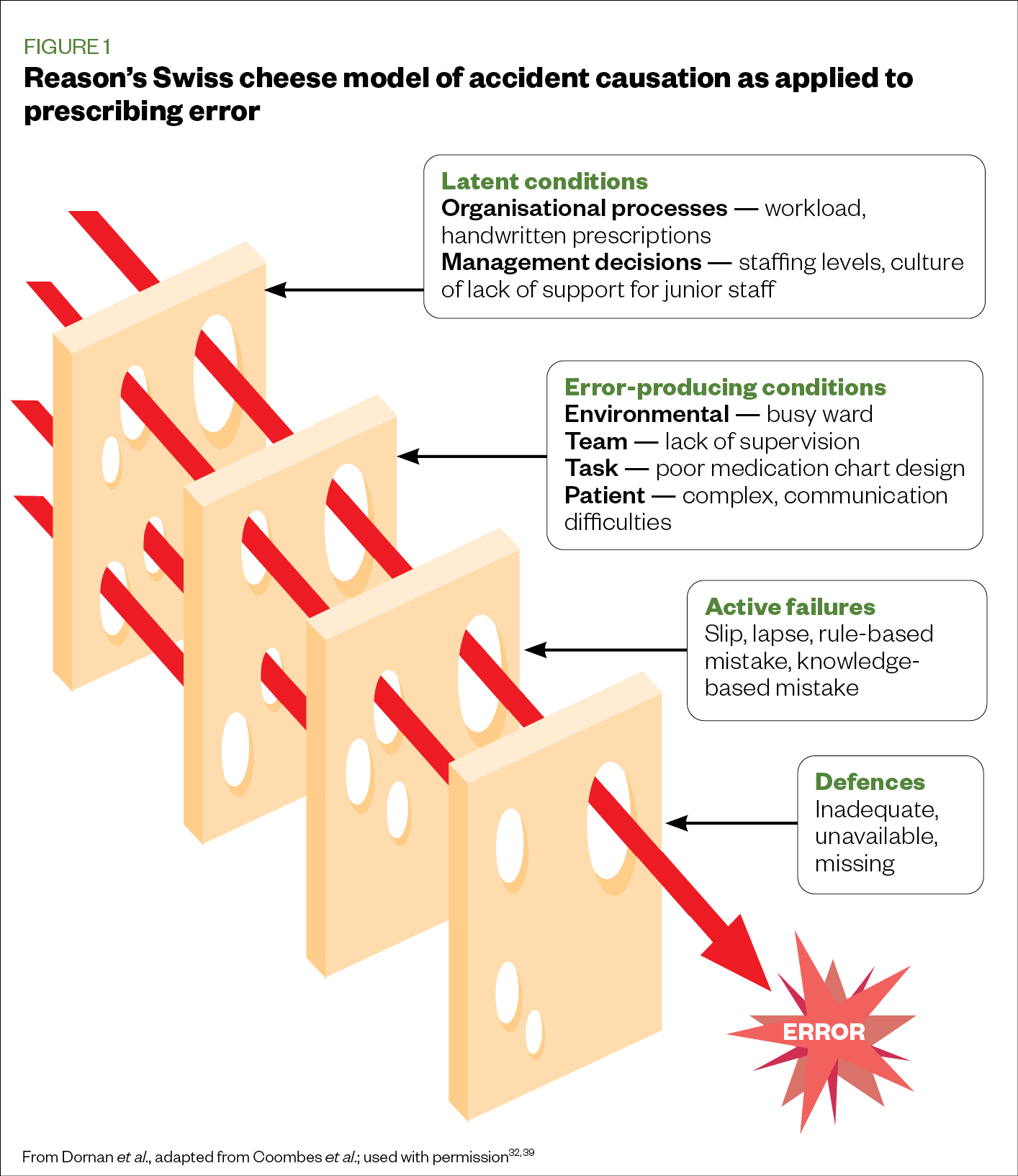
‘The Swiss cheese model’ of accident causation, developed by psychologist James Reason, is the best known theory of error causation in healthcare and has been used to investigate medication errors specifically[37,38]. It contends that systems have multiple layers designed to prevent errors, but that each layer has holes, like Swiss cheese (Figure 1). When these holes align — if problems exist within each layer — errors occur[39].
More recently, focus has shifted onto prescribing behaviour — prescribers’ actions and practices that can lead to error[40]. The Capability-Opportunity-Motivation-Behaviour (COM-B) model contends that, for a behaviour to occur, an individual must have capability, opportunity and motivation[41].
Capability, motivation and opportunity interact with one another: for example, a more capable prescriber might feel more confident and therefore more motivated to complete a task. Alternatively, a practitioner faced with a complex prescription might feel that support is difficult to access (social opportunity), affecting their willingness to seek help and choosing instead to act beyond their limitations (motivation). Analysing this situation using COM-B may prompt consideration of solutions, such as increasing availability of support or the prescriber’s ability to request it, rather than presuming that the prescriber has knowledge deficits that need to be addressed. COM-B’s focus on practitioner behaviour is useful, because supporting individual behaviour change has the potential to impact clinical outcomes.
An example of how the COM-B model (with consideration of task-related factors incorporated) can be applied to a reported error can be seen in Box 1. This approach could be supported by gathering information through conversation with the staff members involved. This sort of analysis guides the response that might be most effective in preventing the same error in future.
For example, in the error outlined in Box 1, training on age and weight-based dosing schedules in paediatrics may be beneficial. This may not be sufficient, however, if prescribers do not see the need to look up resources or feel under too much pressure to do so. In this case, a feedback conversation that helps aid reflection and highlights possible strategies to change behaviour may be helpful. Alternatively, systems changes — such as preventing prescribing during ward rounds and ensuring everyone has access to the digital British National Formulary for Children (published by the Royal Pharmaceutical Society) — may be appropriate. These strategies are not mutually exclusive; in many cases, a multi-pronged approach (e.g. ‘bundle interventions’) will be most effective[41,42].
Box 1: Analysis of a reported error guided by the Capability-Opportunity-Motivation-Behaviour (COM-B) model
A three-day-old baby was prescribed flucloxacillin 62.5mg four times daily for five days. However, the British National Formulary for Children (BNFc) states that for neonates aged under seven days, the dose is 25mg/kg twice daily. When the doctor was contacted, she said she had copied the details from a prescription written by another doctor, and they did not consult the BNFc.
The following was considered from the COM-B model.
Prescribing task:
- Individualised dosing based on age;
- Prescribing for neonates with different dose schedules.
Capability
- Lack of awareness of different dosing schedules;
- Inexperience.
Opportunity:
- Availability of another prescription to copy;
- BNFc may not have been readily to hand, in paper form or via smartphone app;
- Second check/advice may not have been easily accessible.
Motivation:
- Attempting to save time, get the job done quickly without seeking further information;
- Belief that the prescription written by another doctor would be correct.
Behaviour:
- Copying another prescription;
- Prescribing without looking it up.
Causes of prescribing errors in children
Most errors occur in the context of multiple factors, such as haphazard working environments, poor communication, and individual shortcomings[32]. An August 2019 review, which analysed the causes of prescribing errors in children, found that causes of error in adult settings are also likely to apply to paediatric prescribing[24]. The review also demonstrated that prescribing errors in children result from factors specific to prescribing for children[24].
Paediatric-specific causes of errors
Stemming from fundamental differences between children and adults — including variations in size and weight, physiology and metabolism, and pharmacokinetics — the review implicated five paediatric-specific factors in prescribing errors:
- Individualised dosing and calculations;
- Off-licence prescribing;
- Different medication formulations;
- Communication with children and parents;
- Inexperience with working with children[24].
Individualised dosing is the practice of prescribing a specific dose for each patient based on weight, and the consequent requirement to perform calculations; it is the most frequently cited cause of prescribing errors[24]. While individualised dosing is associated with error in adults, the widespread requirement to use this practice in children could contribute to the increased prevalence of paediatric dosing errors[43].
Individualised dosing leads to error in several ways. Prescribers find calculations challenging, often making errors even in controlled classroom settings[44]. Most prescribers appear susceptible, particularly when distracted, contradicting the belief that this represents incompetence within a minority[45]. Some errors occur because some calculations are particularly complex, while others are ‘slips’, such as misplaced decimal points[27]. Errors also happen when prescribers fail to adjust doses as children grow; do not recognise that children are overweight or underweight; or act on incorrect weight measurements[24]. While electronic prescribing (EP) has the potential to prevent errors related to individualised dosing and calculations, evidence suggests that they continue to occur even after its implementation[46].
Off-licence prescribing is a common practice in children, owing to a lack of paediatric evidence regarding medication use[17,47]. While off-licence prescribing is an accepted and necessary part of paediatric practice, evidence shows an association with increased risk of error[47]. Off-licence prescribing places additional responsibilities on prescribers to choose suitable formulations, especially when using extemporaneous preparations — compounding ingredients to prepare an unlicensed medicine for an individual patient in accordance with a prescription — yet clear information on these formulations may be limited[48,49].
The use of different medication formulations is common in paediatric practice, particularly the liquid preparations required for use in younger children[50]. This contributes to errors because prescribers may miscalculate when converting units, such as millilitres to milligrams, or because they choose to prescribe inappropriately by volume instead of weight. This type of error persists because many medications exist in formulations with multiple different strengths, despite efforts to work with pharmaceutical companies to standardise and rationalise concentrations of medicines, and to encourage practitioners to use standardised formulations[51,52].
Risk from these errors is compounded because a volume may seem plausible, yet represent a significant overdose in young children (e.g. a 15mL dose of intravenous paracetamol represents less than one-third of a 50mL vial, but could constitute a tenfold overdose in a 2kg neonate). Besides concentration, prescribers using liquid formulations must also consider issues such as excipient content (phenobarbital liquid, for example, commonly contains a high percentage of alcohol), taste and palatability[48,53]. Other formulation types, primarily designed for use in adults, may have additional considerations: for example, tablets may need to be split, crushed and dispersed to enable administration.
Communication with children and parents may cause errors to arise. This is relevant during medicines reconciliation, when parents sometimes give inaccurate or incomplete information. Children commonly have multiple carers who share responsibility for their medication, particularly when parents live in separate households, which may compound this issue[54]. If an individual states doses only in millilitres, prescribers must establish a correct solution strength and calculate a dose in milligrams[55,56]. Errors may also occur when prescribers change the solution strength of a medication without informing parents (who continue to administer the same volume), or when prescribers verbally inform parents of updated doses, but fail to pass the information on to the child’s GP[57]. These problems may be exacerbated in paediatrics, in which medications are frequently ‘red-listed’, whereby prescribing is retained by the patient’s specialist team rather than their GP[58].
The specific nature of prescribing outlined above may mean that inexperience working with children contributes to errors. For example, errors occur when prescribers more familiar with working with adults prescribe set doses instead of basing them on weight, or rely on memory instead of consulting appropriate resources[59]. This is a common scenario because hospital prescribing for children is sometimes delegated to less experienced junior doctors who undertake the majority of their training in adult settings[32].
These factors show that prescribing for children presents specific challenges for prescribers. Box 2 sets out some practical pitfalls that commonly occur when prescribing for children. Pharmacists should consider the specific challenges in prescribing for children when reviewing prescribed medication, or when analysing errors and providing education and feedback.
Box 2: Paediatric prescribing pitfalls and examples
- Prescribing an overdose for an overweight child by calculating the dose on actual weight rather than age or ideal bodyweight (e.g. prescribing 1g of paracetamol for an obese [70kg] 12-year-old; or prescribing an overdose for an underweight child by using an age-banded dose);
- Performing complex calculations while distracted and without seeking a second check;
- Failing to update doses as children grow and their weight or the dosing schedule changes (e.g. not increasing an anticonvulsant dose based on current weight during the yearly clinic review and therefore not maintaining therapeutic levels);
- Prescribing without a weight or using an incorrect weight;
- Misinterpreting paediatric dosing schedules (e.g. being asked to prescribe an anticonvulsant as 20mg/kg/day in divided doses, but prescribing 20mg/kg twice daily);
- Having difficulty interpreting unclear or competing reference sources for off-licence medications (e.g. between British National Formulary for Children dosing and local policy and guidance);
- Inappropriately prescribing a dose by volume instead of weight, particularly where multiple solution strengths exist (e.g. taking a medication history from a parent and transcribing propranolol 5mL twice daily [of which medicinal forms range from 1mg/mL to 10mg/mL]);
- Making a mistake when converting millilitres to milligrams during medicines reconciliation;
- Failing to communicate medication changes to parents (e.g. changing a preparation to a different strength, but not telling parents that the volume for administration has changed);
- Using set doses from memory instead of looking them up and basing them on age or weight (e.g. prescribing 1.2g of co-amoxiclav for a 30kg 10-year-old);
- Using adult practices when prescribing for a child, such as not using paediatric intravenous fluid rules (e.g. prescribing 1L of intravenous fluid over eight hours for a 14-year-old girl).
Wider causes of errors
There is a lack of primary research on the wider causes of prescribing errors in children; however, two paediatric studies, both published in 2019, point to social, environmental and contextual factors underlying errors.
Bannan et al. studied the causes of prescribing errors on a paediatric oncology ward using the COM-B framework[40]. They found that a mix of factors contributed to errors, including a lack of knowledge, over-reliance on specialist opinions, and the need to balance prescribing with other competing tasks. Sutherland et al. explored the human factors that contributed to prescribing errors in a paediatric intensive care unit[60]. They demonstrated the scale of the prescribing task — finding that 30 subtasks were involved — and proposed that cognitive burden on prescribers was the main factor associated with error. This related to:
- Physical factors, such as fatigue, distractions and interruptions;
- Psychological factors relating to inexperience and a lack of support and information to assist prescribers[60].
Paediatric prescribing errors result from a range of factors, including busy workplace environments, miscommunication, and individuals dealing with highly contextualised and complex tasks, rather than a simple lack of knowledge[32]. This mirrors the findings of the Errors—Questioning Undergraduate Impact on Prescribing (EQUIP) study — one of the first to investigate the underlying causes of prescribing errors in adult practice — which concluded that when an error was caused by a gap in knowledge, it was not the sole cause of the error, and the missing knowledge was complex and contextual rather than the underpinning theory that is taught in undergraduate programmes[32].
While there remains an urgent need for further research (including studies conducted in settings that do not care exclusively for children, such as primary care), the current evidence makes it clear that both paediatric-specific and wider contextual factors that cause errors must be addressed to promote safer paediatric prescribing.
Errors associated with electronic prescribing
EP refers to systems by which prescriptions can be digitally generated and transmitted. They often incorporate clinical decision support (CDS) — computerised systems that can assist prescribers by providing dosing information, issuing warnings or automating calculations. In practice, studies reporting the impact of EP in paediatric hospitals have shown varied results, ranging from a slight increase in mortality to significant decreases in prescribing errors[61–74]. These discrepant results may reflect both the range of different EP systems that are in use and how they are implemented and managed.
Reports of the nature of errors associated with EP from the paediatric population are scarce. Nelson et al. reported on EP errors in a paediatric emergency department, finding that the most common error types were incomplete prescriptions and incorrect dose[75]. A study from a French hospital analysing pharmacist interventions within EP found that lack of patient weight recording and incorrect frequency and dose were the most common errors[76]. These studies suggested that errors related to EP were similar in nature across the paediatric age spectrum. Despite EP’s potential to support practitioners with dose selection and calculations, dosing errors remain common[46].
EP can also introduce new error types. A typical example is prescribers’ tendency to override the frequently occurring warnings offered by CDS systems — so-called ‘alert fatigue’[77]. Moreover, EP systems rely on careful implementation and optimisation. Yet there is no single EP system used in the UK, and most have to support prescribing for all age groups and may lack the specific adaptations — such as mandating weight-dependent dosing — required for paediatric practice[77]. Fox et al. found that when prescribing for children using seven different systems, EP failed to prevent the input of potentially harmful prescription errors in 91% of cases, suggesting that EP cannot be fully relied on to prevent errors despite the additional safeguards it offers[46].
While EP has potential to make prescribing safer (especially in paediatrics where dose assistance and checking could be highly beneficial), it offers only a partial solution. Many of the underlying causes of the errors outlined above — such as distractions, rushing and acting beyond limitations — can apply within EP as much as they do when prescribing by hand. For this reason, it is essential that prescribing safety measures address the specific issues raised by EP and support practitioners in its use, rather than allow it to create a false sense of security.
Independent prescribing
An area showing promise in reducing prescribing errors is independent prescribing by pharmacists and nurse practitioners. The EQUIP study showed that nurse and pharmacist independent prescribers’ error rates were comparable to those of consultants, and lower than those of junior doctors[32]. Another study showed a reduction in errors when a pharmacist independent prescriber was tasked with completing medicines reconciliation and writing drug charts[78].
While further research is needed to assess the impact of independent prescribers in paediatric settings, they have the potential to produce similar benefits in the reduction of error rates. Currently, junior doctors write the majority of prescriptions in secondary care, particularly those required out of hours[32]. While not yet studied empirically, it could be argued that expanding the role of independent prescribers may leave them increasingly susceptible to systemic causes of errors, and could increase their rate of error (and may also impact junior doctors’ capability by reducing their practical experience).
Supporting safer prescribing
Pharmacists support safe prescribing in many ways, including:
- Checking prescriptions in clinical areas or during dispensing;
- Collecting and reviewing audit data;
- Contributing to risk management processes;
- Implementing EP systems;
- Taking part in quality improvement initiatives.
Prescribing education
A particularly important yet potentially overlooked area that can contribute to the prevention of errors is prescribing education. While education makes up a significant portion of pharmacists’ workload, it has been described as ‘low-value intervention’ in promoting patient safety[79]. Similarly, the ‘Hierarchy of Intervention Effectiveness’ — a theory that rates the usefulness of interventions in patient safety used by bodies such as the Institute for Safe Medication Practices — places education at the bottom of the scale[80,81]. Within this classification, human factor solutions, such as automation and forcing functions that make occurrence of errors physically impossible, are strongly preferred[81].
Evidence shows that recent educational approaches, which go beyond raising awareness and focus on behaviour change outcomes, can be effective in addressing prescribing errors[82,83]. Reconceptualising what is thought of as ‘education’, and adopting up-to-date practices based on best evidence, can help to counteract its reputation as a low-value intervention and support safer prescribing.
The complex, multi-factorial nature of prescribing errors in children suggests that educational approaches to error prevention should:
- Be data-driven (incorporating evidence from chart reviews, clinical audits, critical incidents, EP data etc.) and based on an in-depth understanding of how errors happen, generated in collaboration with prescribers and frontline staff[84];
- Be informed by evidence and go beyond increasing knowledge, raising awareness or providing information, and instead focus on changing behaviour[85];
- Be embedded within the working context, not just delivered in classrooms or via electronic learning[32];
- Exist as part of a package of measures, with an ethos of learning and improvement, that promotes a safety culture[86].
Despite the reservations outlined, education — both before and after qualification — remains one of the main ways of promoting safe prescribing, the delivery of which clinical pharmacists are often expected to support. Yet medical students and newly graduated doctors strongly feel that they are not well prepared to prescribe[87]. Most undergraduate prescribing education is ‘off the job’ and relies on simulation, classroom-based training and assessment, rather than experiential learning in context; a survey found that only 35% of medical students had filled in a drug chart more than three times during training[88]. Even after graduation, much prescribing education occurs in classroom settings rather than within practice itself[89]. While these approaches are necessary to develop foundational knowledge, the complex, contextualised nature of prescribing errors means that off-the-job measures alone cannot solve the prescribing safety problem. This is especially true for paediatric prescribing, which places specific demands on prescribers but, owing to congested curricula, receives relatively limited attention within undergraduate training[36].
Therefore, a greater emphasis should be placed on informal educational opportunities that take place within the working context. At undergraduate level, this includes giving medical students the opportunity to prescribe under supervision (including prescribing for children)[90]. In postgraduate practice this could involve giving feedback (discussed in detail below), addressing medication safety issues within multidisciplinary handovers, or discussing prescribing decisions during ward rounds. Measures such as these, which seek the involvement of a wide range of stakeholders and promote shared decision-making, have the potential to go beyond individual development and positively impact workplace culture. Pharmacists might also consider how they can be available to support prescribers’ education during prescribing — a process known as ‘feedforward’ — including those looking after children in clinical areas without formal paediatric pharmacy cover.
More formal learning opportunities, which could include prescribing workshops, practice calculations and simulated prescribing scenarios, should augment this approach. The content of these should focus on practical aspects of prescribing — considering the causes of errors — and respond to real-life issues and requests from prescribers. Induction processes, particularly for prescribers who have not worked with children before, should outline paediatric-specific prescribing practices and offer specific advice on performing calculations. Formally testing individuals or restricting prescribing responsibility to certain groups, however, is unlikely to be helpful (although there may be individuals, such as those who have specific difficulties with calculations, who should be offered a greater level of support). Recently developed online resources, such as the eLearning programme Paediatric SCRIPT and those offered by the Royal College of Paediatrics and Child Health, may be useful to support these approaches[91,92].
Prescribing feedback
Described as ‘the cornerstone of effective clinical teaching’, feedback has the potential to support prescribers’ ongoing professional development and prescribing performance. Feedback works by raising self-awareness, encouraging reflection and reducing the gap between perceived and actual performance[93–95]. A growing body of evidence underpins its use, with systematic reviews suggesting that feedback can have small but important impacts on professional practice, particularly when targeting outcomes such as safe prescribing[96–98]. In paediatrics specifically, feedback interventions have reduced prescribing errors[99–102]. Professional bodies including the Royal Pharmaceutical Society and the Royal College of Physicians have stressed the importance of prescribing feedback, especially for junior doctors[13,103].
In practice, learners often complain that feedback is insufficient, infrequent or of low quality[94,104]. In particular, prescribers have reported a lack of feedback on, and awareness of, their own prescribing errors[32,105–107]. In many cases (83% of detected errors in one study), hospital pharmacists correct errors without informing the prescriber[19,108]. This approach, while maintaining safety in the short term, can be seen as a missed learning opportunity. Where feedback is absent, limited, or of poor quality, prescribers may develop false perceptions that they are performing well and continue making the same prescribing errors at the expense of patient safety[109].
Box 3: Example structure of a feedback conversation
Based on the error outlined in Box 1, in which a prescriber copied another doctor’s prescription rather than checking resources or asking for advice, a feedback conversation might include the following points.
Discuss the error non-judgementally and clarify any details.
Ask questions, encouraging the prescriber to reflect on their prescribing behaviour (which can be guided by the frameworks outlined previously):
- “Were there any gaps in your knowledge that may have contributed?”, perhaps eliciting lack of experience of prescribing for neonates and calculating doses;
- “Were there external features that made you act in the way that you did?”, may highlight that resources and people to ask for help were not readily available;
- “What made you decide to prescribe when you felt unsure?”, perhaps eliciting the desire to save time or the assumptions that the previous prescription was correct.
Based on the discussion, ask the prescriber to reflect on how they could act differently to prevent similar errors; enquire whether changes could be put in place to support them in doing so.
Ask the prescriber if there are behaviour changes that they could implement based on the feedback conversation.
What should feedback look like?
Feedback is an essential resource for promoting prescribing safety, and opportunities to deliver it should be increased. While most pharmacists interact with prescribers on daily basis, there is debate about what interactions should be considered feedback. A recent definition describes feedback as a process in which individuals receive information about their work, enabling them to compare it with best practice and think about how they might improve it in future[110]. Others have argued, however, that providing information, especially in the form of grades, ratings or written comments, does not on its own constitute feedback[111]. Instead, they contend that feedback needs to involve a two-way conversation during which shared understandings or solutions can be developed[111]. This article proposes that practitioners involved in delivering feedback to learners should aspire to the latter definition because it is more likely to lead to meaningful changes in practice.
To deliver this sort of feedback in practice, educators should consider both the conditions under which feedback is given and the feedback process itself[94,109,112]. Systematic reviews have reported that effective feedback should be timely, frequent and integrated into routine practice[96–98]. Feedback is best facilitated by a colleague in a setting conducive to relaxed and open discussion, with verbal delivery supported by written information[11,109]. Doctors consider pharmacists, who work closely with them on hospital wards and routinely observe their prescribing, as well-placed to deliver prescribing feedback[11,105,113]. The feedback process can be either directive or facilitative[114]:
- Directive feedback simply informs the learner of the required correction via a monologue in which the learner is a passive recipient. Pharmacists acknowledge that, while a common routine process of correcting prescribing errors, it is unlikely to change prescribing practice[109];
- Facilitative feedback is a constructive and dynamic process in which the facilitator uses open questions and comments to help learners understand and revise their own prescribing decisions and practices[114]. It begins by seeking the prescriber’s understanding of the situation and what caused it, and focuses on prescribing performance in relation to specific events rather than prescribers’ overall competence or personal characteristics.
The ‘data’ to inform these discussions can come from errors identified in routine practice, through incident reporting, or may be offered by prescribers themselves. Facilitative feedback leads to negotiated, prescriber-specific action plans, emphasising commitments to behaviour change[115]. As facilitative feedback involves a discussion about errors’ underlying causes, it should also remain open to solutions beyond the individual prescriber, such as system changes. Together, these features mean that facilitative feedback enables reflective practice, an essential component of prescribing[13], and has the potential to shape future prescribing practice rather than just raising awareness[116]. This description highlights that giving feedback is a learned skill that requires practice and reflection. Table 2 offers practical tips to help practitioners hoping to improve how they facilitate prescribing feedback.
Challenges
While the approaches outlined are based on evidence and represent current best practice, barriers exist to their implementation. Analysing errors, delivering education and giving feedback are time-consuming processes that require specific skills and experience. This is a particularly important issue because many children are looked after in clinical areas that may not have dedicated paediatric pharmacist provision[117]. Ultimately, additional staff — such as paediatric clinical pharmacists, medication safety officers, and education and training pharmacists — will be needed for improvements to be fully realised.
Nonetheless, many of the principles outlined can be integrated into pharmacists’ existing role and workload. For example, there may be more benefit in prioritising a smaller number of in-depth feedback conversations rather than flagging every incorrect prescription. Similarly, only some errors, based on risk and their potential to inform improvement, need be analysed in detail. Other errors could be discussed more briefly, during opportunities such as handovers. Reported errors can be used effectively in aggregate[30].
These approaches, all of which are intended to emphasise learning rather than apportion individual responsibility, may result in the promotion of a safety culture. It is recognised that many of these approaches apply in frontline hospital settings, but may be more difficult to implement when errors are detected in dispensaries or community pharmacies. While a working knowledge of common paediatric prescribing errors may support error detection, giving prescribers education or feedback may be outside the remit of community pharmacists. In these cases, liaising with the relevant hospital or primary care pharmacist may be appropriate. Additionally, opportunities for community pharmacists and primary care colleagues to meet as part of continuing professional development are likely to be helpful[118].
Box 4: Best practice for pharmacists aiming to promote safer prescribing for children
- Prioritise high-risk error types, medications, patient groups and areas of practice, where possible guided by data from within local practice;
- When designing paediatric education, consider both paediatric-specific and generic causes of errors, including individualised dosing, calculations and prescribers’ level of experience;
- Use frameworks to support detailed analysis of the systemic causes of errors, such as the Swiss cheese model or the Capability-Opportunity-Motivation-Behaviour framework;
- Select the most effective approach for preventing errors based on their underlying causes;
- Consider complementary interventions for different error types;
- Emphasise informal educational opportunities within practice rather than classroom teaching;
- Make behaviour change the target of education and quality improvement interventions, not just the provision of information;
- Use a facilitative style of feedback to help prescribers reflect on their prescribing and commit to meaningful changes in practice;
- Explicitly and deliberately emphasise errors’ potential to stimulate learning within teams rather than apportioning individual responsibility;
- Carefully consider how electronic prescribing systems are adapted for use in children and give prescribers practical support in their use.
This article was has been reviewed by the expert authors to ensure it remains relevant and up-to-date, following its original publication in The Pharmaceutical Journal in March 2021.
- 1Carson-Stevens A, Edwards A, Panesar S, et al. Reducing the burden of iatrogenic harm in children. The Lancet 2015;:1593–4. doi:10.1016/s0140-6736(14)61739-6
- 2Ghaleb MA, Barber N, Franklin BD, et al. The incidence and nature of prescribing and medication administration errors in paediatric inpatients. Archives of Disease in Childhood 2010;:113–8. doi:10.1136/adc.2009.158485
- 3Cousins D, Clarkson A, Conroy S, et al. Medication Errors in Children – an Eight Year Review Using Press Reports. Paediatric and Perinatal Drug Therapy 2002;:52–8. doi:10.1185/146300902322125893
- 4Alenezi S, Abramson J, Smith C, et al. INTERVENTIONS MADE BY UK PHARMACISTS TO MINIMISE RISK FROM PAEDIATRIC PRESCRIBING ERRORS. Arch Dis Child 2016;:e2.62-e2. doi:10.1136/archdischild-2016-311535.65
- 5Kaushal R, Bates D, Landrigan C. Medication Errors and Adverse Drug Events in Pediatric Inpatients. Survey of Anesthesiology 2001;285:2114–20. doi:10.1001/jama.285.16.2114
- 6Donaldson LJ, Kelley ET, Dhingra-Kumar N, et al. Medication Without Harm: WHO’s Third Global Patient Safety Challenge. The Lancet 2017;:1680–1. doi:10.1016/s0140-6736(17)31047-4
- 7Tully MP. Prescribing errors in hospital practice. British Journal of Clinical Pharmacology 2012;:668–75. doi:10.1111/j.1365-2125.2012.04313.x
- 8Cass H. Reducing paediatric medication error through quality improvement networks; where evidence meets pragmatism. Arch Dis Child 2016;:414–6. doi:10.1136/archdischild-2015-309007
- 9Sanghera N, Chan P-Y, Khaki ZF, et al. Interventions of Hospital Pharmacists in Improving Drug Therapy in Children. Drug Safety 2006;:1031–47. doi:10.2165/00002018-200629110-00003
- 10Preslaski CR, Lat I, MacLaren R, et al. Pharmacist Contributions as Members of the Multidisciplinary ICU Team. Chest 2013;:1687–95. doi:10.1378/chest.12-1615
- 11Lloyd M, Watmough S, O’Brien S, et al. Formalized prescribing error feedback from hospital pharmacists: doctors’ attitudes and opinions. British Journal of Hospital Medicine 2015;:713–8. doi:10.12968/hmed.2015.76.12.713
- 12Al-Kudhairi F, Kayyali R, Savickas V, et al. A Qualitative Study Exploring the Role of Pharmacists in Medical Student Training for the Prescribing Safety Assessment. Pharmacy 2018;:87. doi:10.3390/pharmacy6030087
- 13Framework for All Prescribers. Royal Pharmaceutical Society. 2016.https://www.rpharms.com/Portals/0/RPS document library/Open access/Professional standards/Prescribing competency framework/prescribing-competency-framework.pdf (accessed Jan 2021).
- 14Good Practice in Prescribing and Managing Medicines and Devices. General Medical Council. 2013.https://www.gmc-uk.org/-/media/documents/prescribing-guidance_pdf-59055247.pdf (accessed Jan 2021).
- 15Dean B. What is a prescribing error? Quality in Health Care 2000;:232–7. doi:10.1136/qhc.9.4.232
- 16Ghaleb MA. What constitutes a prescribing error in paediatrics? Quality and Safety in Health Care 2005;:352–7. doi:10.1136/qshc.2005.013797
- 17Ekins-Daukes S, Helms PeterJ, Simpson ColinR, et al. Off-label prescribing to children in primary care: retrospective observational study. Eur J Clin Pharmacol Published Online First: 14 May 2004. doi:10.1007/s00228-004-0752-1
- 18Wilson DG, McArtney RG, Newcombe RG, et al. Medication errors in paediatric practice: insights from a continuous quality improvement approach. European Journal of Pediatrics 1998;:769–74. doi:10.1007/s004310050932
- 19Olsen S, Neale G, Schwab K, et al. Hospital staff should use more than one method to detect adverse events and potential adverse events: incident reporting, pharmacist surveillance and local real-time record review may all have a place. Quality and Safety in Health Care 2007;:40–4. doi:10.1136/qshc.2005.017616
- 20Simpson JH. Reducing medication errors in the neonatal intensive care unit. Archives of Disease in Childhood – Fetal and Neonatal Edition 2004;:F480–2. doi:10.1136/adc.2003.044438
- 21Elliott R, Camacho E, Campbell F et al. Prevalence and Economic Burden of Medication Errors in the NHS in England. Economic Methods of Evaluation of Health and Social Care Interventions. 2018.http://www.eepru.org.uk/prevalence-and-economic-burden-of-medication-errors-in-the-nhs-in-england-2/ (accessed Jan 2021).
- 22Wu AW. Medical error: the second victim. BMJ 2000;:726–7. doi:10.1136/bmj.320.7237.726
- 23Dangerous Abbreviations list. National Coordinating Council for Medication Error Reporting and Prevention. 2021.https://www.nccmerp.org/dangerous-abbreviations (accessed Jan 2021).
- 24Conn RL, Kearney O, Tully MP, et al. What causes prescribing errors in children? Scoping review. BMJ Open 2019;:e028680. doi:10.1136/bmjopen-2018-028680
- 25Wong ICK, Ghaleb MA, Franklin BD, et al. Incidence and Nature of Dosing Errors in Paediatric Medications. Drug Safety 2004;:661–70. doi:10.2165/00002018-200427090-00004
- 26Review of patient safety for children and young people. National Patient Safety Agency. 2009.https://webarchive.nationalarchives.gov.uk/20090703113024/http://www.npsa.nhs.uk/nrls/improvingpatientsafety/children-and-young-people/ (accessed Jan 2021).
- 27Lesar TS. Tenfold Medication Dose Prescribing Errors. Ann Pharmacother 2002;:1833–9. doi:10.1345/aph.1c032
- 28Battles JB. Organizing patient safety research to identify risks and hazards. Quality and Safety in Health Care 2003;:2ii–7. doi:10.1136/qhc.12.suppl_2.ii2
- 29NCC MERP Index for Categorizing Medication Errors. National Coordinating Council for Medication Error Reporting and Prevention. 2001.https://www.nccmerp.org/sites/default/files/indexColor2001-06-12.pdf (accessed Jan 2021).
- 30Conn RL, Tully MP, Shields MD, et al. Characteristics of Reported Pediatric Medication Errors in Northern Ireland and Use in Quality Improvement. Pediatr Drugs 2020;:551–60. doi:10.1007/s40272-020-00407-1
- 31Noble DJ, Pronovost PJ. Underreporting of Patient Safety Incidents Reduces Health Care’s Ability to Quantify and Accurately Measure Harm Reduction. Journal of Patient Safety 2010;:247–50. doi:10.1097/pts.0b013e3181fd1697
- 32Dornan T, Ashcroft D, Lewis P et al. An in Depth Investigation into Causes of Prescribing Errors by Foundation Trainees in Relation to Their Medical Education – EQUIP Study. General Medical Council. 2009.http://www.gmc-uk.org/FINAL_Report_prevalence_and_causes_of_prescribing_errors.pdf_28935150.pdf (accessed Jan 2021).
- 33High-Alert Medications in Acute Care Settings. Institute for Safe Medication Practices. 2018. https://www.ismp.org/recommendations/high-alert-medications-acute-list (accessed Jan 2021).
- 34Shaw KN, Lillis KA, Ruddy RM, et al. Reported medication events in a paediatric emergency research network: sharing to improve patient safety. Emerg Med J 2012;:815–9. doi:10.1136/emermed-2012-201642
- 35Conroy S, Sweis D, Planner C, et al. Interventions to Reduce Dosing Errors in Children. Drug Safety 2007;:1111–25. doi:10.2165/00002018-200730120-00004
- 36Conroy S, Carroll WD. Prescribing in paediatrics. Archives of Disease in Childhood – Education and Practice 2009;:55–9. doi:10.1136/adc.2008.141754
- 37Reason J. Human error: models and management. BMJ 2000;:768–70. doi:10.1136/bmj.320.7237.768
- 38Tully MP, Ashcroft DM, Dornan T, et al. The Causes of and Factors Associated with Prescribing Errors in Hospital Inpatients. Drug Safety 2009;:819–36. doi:10.2165/11316560-000000000-00000
- 39Coombes ID, Stowasser DA, Coombes JA, et al. Why do interns make prescribing errors? A qualitative study. Medical Journal of Australia 2008;:89–94. doi:10.5694/j.1326-5377.2008.tb01529.x
- 40Bannan DF, Aseeri MA, AlAzmi A, et al. Understanding the causes of prescribing errors from a behavioural perspective. Research in Social and Administrative Pharmacy 2019;:546–57. doi:10.1016/j.sapharm.2018.07.007
- 41Michie S, van Stralen MM, West R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implementation Sci Published Online First: 23 April 2011. doi:10.1186/1748-5908-6-42
- 42Bannan DF, Tully MP. Bundle interventions used to reduce prescribing and administration errors in hospitalized children: a systematic review. J Clin Pharm Ther 2016;:246–55. doi:10.1111/jcpt.12398
- 43Rapid Response Report: NPSA/2010/RRR014: Reducing treatment dose errors with low molecular weight heparins. National Patient Safety Agency. 2010.https://www.sps.nhs.uk/wp-content/uploads/2018/02/2010-NRLS-1270-LMWH-Supportingmation-2010.10.11-v2.pdf (accessed Jan 2021).
- 44Menon L, Taylor Z, Tuthill DP. Can paediatric junior hospital doctors prescribe competently? Paediatric and Perinatal Drug Therapy 2006;:118–20. doi:10.1185/146300906×105168
- 45Glover ML, Sussmane JB. Assessing Pediatrics Residentsʼ Mathematical Skills for Prescribing Medication. Academic Medicine 2002;:1007–10. doi:10.1097/00001888-200210000-00013
- 46Fox A, Portlock J, Brown D. Electronic prescribing in paediatric secondary care: are harmful errors prevented? Arch Dis Child 2019;:895–9. doi:10.1136/archdischild-2019-316859
- 47Conroy S. Association between licence status and medication errors. Archives of Disease in Childhood 2010;:305–6. doi:10.1136/adc.2010.191940
- 48Choosing an Oral Liquid Medicine for Children. Neonatal & Paediatric Pharmacists Group. 2020.http://nppg.org.uk/wp-content/uploads/2020/12/Position-Statement-Liquid-Choice-V1-November-2020.pdf (accessed Jan 2021).
- 49McCague P, McElnay J, Donnelly R. What are your views on specials and extemporaneous medicines preparation? . Pharm J 2012;288:722.
- 50Mani V, Wheeler DW. Drug Form and Expression of Concentration May also Lead to Prescription Errors. Drug Safety 2010;:167–8. doi:10.2165/11319060-000000000-00000
- 51Sullivan JE, Buchino JJ. Medication errors in pediatrics?the octopus evading defeat. J Surg Oncol 2004;:182–8. doi:10.1002/jso.20126
- 52Using Standardised Strengths of Unlicensed Liquid Medicines in Children. Neonatal & Paediatric Pharmacists Group. 2018. http://nppg.org.uk/wp-content/uploads/2020/04/NPPG-Position-Statement-18-01-V5-April-2020.pdf (accessed Jan 2021).
- 53Baguley D, Lim E, Bevan A, et al. Prescribing for children – taste and palatability affect adherence to antibiotics: a review. Arch Dis Child 2011;:293–7. doi:10.1136/archdischild-2011-300909
- 54Riley-Lawless K. Family-Identified Barriers to Medication Reconciliation. Journal for Specialists in Pediatric Nursing 2009;:94–101. doi:10.1111/j.1744-6155.2009.00182.x
- 55Lesar TS, Mitchell A, Sommo P. Medication Safety in Critically Ill Children. Clinical Pediatric Emergency Medicine 2006;:215–25. doi:10.1016/j.cpem.2006.08.009
- 56Hughes RG, Edgerton EA. Reducing Pediatric Medication Errors. AJN, American Journal of Nursing 2005;:79–84. doi:10.1097/00000446-200505000-00035
- 57Diav-Citrin O, Ratnapalan S, Grouhi M, et al. Medication Errors in Paediatrics. Paediatric Drugs 2000;:239–42. doi:10.2165/00128072-200002030-00007
- 58Guidelines on defining RED/AMBER/GREEN/MEDICINE Status. Greater Manchester Medicines Management Group. 2014.http://gmmmg.nhs.uk/docs/ip/Guidelines on defining RED AMBER GREEN STATUS June 14.pdf (accessed Jan 2021).
- 59Conn RL, McVea S, Carrington A, et al. Intravenous fluid prescribing errors in children: Mixed methods analysis of critical incidents. PLoS ONE 2017;:e0186210. doi:10.1371/journal.pone.0186210
- 60Sutherland A, Ashcroft DM, Phipps DL. Exploring the human factors of prescribing errors in paediatric intensive care units. Arch Dis Child 2019;:588–95. doi:10.1136/archdischild-2018-315981
- 61Han YY. Unexpected Increased Mortality After Implementation of a Commercially Sold Computerized Physician Order Entry System. PEDIATRICS 2005;:1506–12. doi:10.1542/peds.2005-1287
- 62Del Beccaro MA, Jeffries HE, Eisenberg MA, et al. Computerized Provider Order Entry Implementation: No Association With Increased Mortality Rates in an Intensive Care Unit. PEDIATRICS 2006;:290–5. doi:10.1542/peds.2006-0367
- 63Kadmon G, Bron-Harlev E, Nahum E, et al. Computerized Order Entry With Limited Decision Support to Prevent Prescription Errors in a PICU. PEDIATRICS 2009;:935–40. doi:10.1542/peds.2008-2737
- 64Kazemi A, Ellenius J, Pourasghar F, et al. The Effect of Computerized Physician Order Entry and Decision Support System on Medication Errors in the Neonatal Ward: Experiences from an Iranian Teaching Hospital. J Med Syst 2009;:25–37. doi:10.1007/s10916-009-9338-x
- 65Sullins AK, Richard AA, Manasco KB, et al. Which Comes First CPOE or eMAR? A Retrospective Analysis of Health Information Technology Implementation. Hospital Pharmacy 2012;:863–70. doi:10.1310/hpj4711-863
- 66O’Meara M, Shaheen N. ELECTRONIC PRESCRIBING: FRIEND OR FOE? AN AUDIT OF PRESCRIBING ERRORS AFTER THE INTRODUCTION OF AN ELECTRONIC PRESCRIBING SYSTEM IN NEONATES AND CHILDREN. Archives of Disease in Childhood 2014;:e3–e3. doi:10.1136/archdischild-2014-306798.2
- 67Keene A, Ashton L, Shure D, et al. Mortality before and after initiation of a computerized physician order entry system in a critically ill pediatric population*. Pediatric Critical Care Medicine 2007;:268–71. doi:10.1097/01.pcc.0000260781.78277.d9
- 68Longhurst CA, Parast L, Sandborg CI, et al. Decrease in Hospital-wide Mortality Rate After Implementation of a Commercially Sold Computerized Physician Order Entry System. PEDIATRICS 2010;:14–21. doi:10.1542/peds.2009-3271
- 69King WJ, Paice N, Rangrej J, et al. The Effect of Computerized Physician Order Entry on Medication Errors and Adverse Drug Events in Pediatric Inpatients. PEDIATRICS 2003;:506–9. doi:10.1542/peds.112.3.506
- 70Cordero L, Kuehn L, Kumar RR, et al. Impact of Computerized Physician Order Entry on Clinical Practice in a Newborn Intensive Care Unit. J Perinatol 2004;:88–93. doi:10.1038/sj.jp.7211000
- 71Potts AL, Barr FE, Gregory DF, et al. Computerized Physician Order Entry and Medication Errors in a Pediatric Critical Care Unit. PEDIATRICS 2003;:59–63. doi:10.1542/peds.113.1.59
- 72Upperman JS, Staley P, Friend K, et al. The impact of hospitalwide computerized physician order entry on medical errors in a pediatric hospital. Journal of Pediatric Surgery 2005;:57–9. doi:10.1016/j.jpedsurg.2004.09.024
- 73Holdsworth MT, Fichtl RE, Raisch DW, et al. Impact of Computerized Prescriber Order Entry on the Incidence of Adverse Drug Events in Pediatric Inpatients. PEDIATRICS 2007;:1058–66. doi:10.1542/peds.2006-3160
- 74Walsh KE, Landrigan CP, Adams WG, et al. Effect of Computer Order Entry on Prevention of Serious Medication Errors in Hospitalized Children. PEDIATRICS 2008;:e421–7. doi:10.1542/peds.2007-0220
- 75Nelson CE, Selbst SM. Electronic Prescription Writing Errors in the Pediatric Emergency Department. Pediatric Emergency Care 2015;:368–72. doi:10.1097/pec.0000000000000428
- 76Alhanout K, Bun S-S, Retornaz K, et al. Prescription errors related to the use of computerized provider order-entry system for pediatric patients. International Journal of Medical Informatics 2017;:15–9. doi:10.1016/j.ijmedinf.2017.04.005
- 77Sutcliffe K, Stokes G, Caird J et al. Paediatric Medication Error: A Systematic Review of the Extent and Nature of the Problem in the UK and International Interventions to Address It. EPPI-Centre. 2014.https://eppi.ioe.ac.uk/cms/Portals/0/PDF%20reviews%20and%20summaries/Paediatric%20medication%20error%202014%20Sutcliffe%20report.pdf?ver=2014-11-20-161504-377 (accessed Jan 2021).
- 78Mills PR, McGuffie AC. Formal medicine reconciliation within the emergency department reduces the medication error rates for emergency admissions. Emergency Medicine Journal 2010;:911–5. doi:10.1136/emj.2009.082255
- 79Soong C, Shojania KG. Education as a low-value improvement intervention: often necessary but rarely sufficient. BMJ Qual Saf 2019;:353–7. doi:10.1136/bmjqs-2019-010411
- 80Key Definitions. Institute for Safe Medication Practices. 2021.https://mssa.ismp-canada.org/homecareorg1/page/50 (accessed Jan 2021).
- 81Woods DM, Holl JL, Angst D et al. Improving Clinical Communication and Patient Safety: Clinician-Recommended Solutions. In: Henriksen K, Battles JB, Keyes MA et al, ed. Advances in Patient Safety: New Directions and Alternative Approaches . Rockville (MD): : Agency for Healthcare Research and Quality 2008. (Vol. 3: Performance and Tools).
- 82McLellan L, Dornan T, Newton P, et al. Pharmacist-led feedback workshops increase appropriate prescribing of antimicrobials. J Antimicrob Chemother 2016;:1415–25. doi:10.1093/jac/dkv482
- 83Parker H, Farrell O, Bethune R, et al. Pharmacist‐led, video‐stimulated feedback to reduce prescribing errors in doctors‐in‐training: A mixed methods evaluation. Br J Clin Pharmacol 2019;:2405–13. doi:10.1111/bcp.14065
- 84Rees P, Carson-Stevens A, Williams H, et al. Quality improvement informed by a reporting and learning system. Archives of Disease in Childhood 2014;:702–3. doi:10.1136/archdischild-2014-306198
- 85Brennan N, Mattick K. A systematic review of educational interventions to change behaviour of prescribers in hospital settings, with a particular emphasis on new prescribers. Br J Clin Pharmacol 2013;:359–72. doi:10.1111/j.1365-2125.2012.04397.x
- 86Dekker S. Failure to adapt or adaptations that fail: contrasting models on procedures and safety. Applied Ergonomics 2003;:233–8. doi:10.1016/s0003-6870(03)00031-0
- 87Monrouxe LV, Bullock A, Gormley G, et al. New graduate doctors’ preparedness for practice: a multistakeholder, multicentre narrative study. BMJ Open 2018;:e023146. doi:10.1136/bmjopen-2018-023146
- 88Heaton A, Webb DJ, Maxwell SRJ. Undergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol 2008;:128–34. doi:10.1111/j.1365-2125.2008.03197.x
- 89Conroy S, North C, Fox T, et al. Educational interventions to reduce prescribing errors. Archives of Disease in Childhood 2008;:313–5. doi:10.1136/adc.2007.127761
- 90Gillespie H, McCrystal E, Reid H, et al. The pen is mightier than the sword. Reinstating patient care as the object of prescribing education. Medical Teacher 2020;:50–7. doi:10.1080/0142159x.2020.1795103
- 91Paediatric SCRIPT. University of Birmingham/OCB Media. 2016.https://www.safeprescriber.org/paediatric (accessed Jan 2021).
- 92Paediatric prescribing principles. Royal College of Paediatrics and Child Health. 2016. https://www.rcpch.ac.uk/resources/paediatric-prescribing-principles-online-learning (accessed Jan 2021).
- 93Hesketh EA, Laidlaw JM. Developing the teaching instinct, 1: Feedback. Medical Teacher 2002;:245–8. doi:10.1080/014215902201409911
- 94Cantillon P, Sargeant J. Giving feedback in clinical settings. BMJ 2008;:a1961–a1961. doi:10.1136/bmj.a1961
- 95Randolph G, Esporas M, Provost L, et al. Model for Improvement – Part Two: Measurement and Feedback for Quality Improvement Efforts. Pediatric Clinics of North America 2009;:779–98. doi:10.1016/j.pcl.2009.05.012
- 96Jamtvedt G, Young JM, Kristoffersen DT, et al. Does telling people what they have been doing change what they do? A systematic review of the effects of audit and feedback. Quality and Safety in Health Care 2006;:433–6. doi:10.1136/qshc.2006.018549
- 97Ivers NM, Grimshaw JM, Jamtvedt G, et al. Growing Literature, Stagnant Science? Systematic Review, Meta-Regression and Cumulative Analysis of Audit and Feedback Interventions in Health Care. J GEN INTERN MED 2014;:1534–41. doi:10.1007/s11606-014-2913-y
- 98Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database of Systematic Reviews Published Online First: 13 June 2012. doi:10.1002/14651858.cd000259.pub3
- 99Booth R, Sturgess E, Taberner-Stokes A, et al. Zero tolerance prescribing: a strategy to reduce prescribing errors on the paediatric intensive care unit. Intensive Care Med 2012;:1858–67. doi:10.1007/s00134-012-2660-7
- 100Sullivan KM, Suh S, Monk H, et al. Personalised performance feedback reduces narcotic prescription errors in a NICU. BMJ Qual Saf 2012;:256–62. doi:10.1136/bmjqs-2012-001089
- 101Eisenhut M, Sun B, Skinner S. Reducing Prescribing Errors in Paediatric Patients by Assessment and Feedback Targeted at Prescribers. ISRN Pediatrics 2011;:1–5. doi:10.5402/2011/545681
- 102Wyllie T. SP6 Building on the druggle: personalised feedback to improve and maintain good prescribing practice. Arch Dis Child 2020;:e3.2-e4. doi:10.1136/archdischild-2020-nppg.6
- 103Supporting junior doctors in safe prescribing. Royal College of Physicians. 2017.https://www.rcplondon.ac.uk/projects/outputs/supporting-junior-doctors-safe-prescribing (accessed Jan 2021).
- 104Pelgrim EAM, Kramer AWM, Mokkink HGA, et al. The process of feedback in workplace-based assessment: organisation, delivery, continuity. Medical Education 2012;:604–12. doi:10.1111/j.1365-2923.2012.04266.x
- 105Bertels J, Almoudaris AM, Cortoos P-J, et al. Feedback on prescribing errors to junior doctors: exploring views, problems and preferred methods. Int J Clin Pharm 2013;:332–8. doi:10.1007/s11096-013-9759-y
- 106Lewis PJ, Ashcroft DM, Dornan T, et al. Exploring the causes of junior doctors’ prescribing mistakes: a qualitative study. Br J Clin Pharmacol 2014;:310–9. doi:10.1111/bcp.12332
- 107Lloyd M, Watmough SD, O’Brien SV, et al. Exploring the impact of pharmacist-led feedback on prescribing behaviour: A qualitative study. Research in Social and Administrative Pharmacy 2018;:545–54. doi:10.1016/j.sapharm.2017.06.010
- 108Abdel-Qader DH, Harper L, Cantrill JA, et al. Pharmacistsʼ Interventions in Prescribing Errors at Hospital Discharge. Drug Safety 2010;:1027–44. doi:10.2165/11538310-000000000-00000
- 109Lloyd M, Watmough SD, O’Brien SV, et al. Exploring attitudes and opinions of pharmacists toward delivering prescribing error feedback: A qualitative case study using focus group interviews. Research in Social and Administrative Pharmacy 2016;:461–74. doi:10.1016/j.sapharm.2015.08.012
- 110Boud D, Molloy E. What Is the Problem with Feedback? Feedback in Higher and Professional Education: Understanding It and Doing It Well. 1st ed. London: : Routledge 2013.
- 111Ajjawi R, Regehr G. When I say … feedback. Med Educ 2018;:652–4. doi:10.1111/medu.13746
- 112Ramani S, Krackov SK. Twelve tips for giving feedback effectively in the clinical environment. Medical Teacher 2012;:787–91. doi:10.3109/0142159x.2012.684916
- 113Lloyd M, Watmough SD, O’Brien SV, et al. Exploring the impact of feedback on prescribing error rates: a pilot study. Int J Clin Pharm 2017;:1013–7. doi:10.1007/s11096-017-0503-x
- 114Archer JC. State of the science in health professional education: effective feedback. Medical Education 2010;:101–8. doi:10.1111/j.1365-2923.2009.03546.x
- 115Bing-You R, Varaklis K, Hayes V, et al. The Feedback Tango. Academic Medicine 2018;:657–63. doi:10.1097/acm.0000000000001927
- 116Sargeant JM, Mann KV, van der Vleuten CP, et al. Reflection: a link between receiving and using assessment feedback. Adv in Health Sci Educ 2008;:399–410. doi:10.1007/s10459-008-9124-4
- 117Webster S, Kane C, Brown C, et al. Pediatric Pharmacy Services: Current Models and Justification for Expansion. The Journal of Pediatric Pharmacology and Therapeutics 2019;:438–44. doi:10.5863/1551-6776-24.5.438
- 118New partnership signals exciting development opportunity for community pharmacists. Royal College of General Practitioners. 2020.https://www.rcgp.org.uk/about-us/news/2020/september/new-partnership-signals-exciting-development-opportunity-for-community-pharmacists.aspx (accessed Jan 2021).